Malarial Parasites Investigation (Blood films and Rapid Diagnostic Test)
Specimen Volume
4mLSpecimen Transport
Standard transport to laboratorySample Preparation
Turnaround Time
24 hours, if urgent by prior arrangement with laboratorySample Stability
4°C for 24 hour (Blood Film) or 72 hours (Rapid Diagnostic Test only)General Information
Microscopy and antigen detection for malarial parasites can be performed on the same sample as the FBC sample. Please supply details of which countries the patient has visited along with prophylaxis or treatment details.
All malaria requests now incorporate the malaria antigen test in addition to microscopy.
Notes
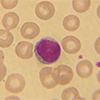
Blood Film
Thin Blood films are stained at pH7.2 with Giemsa and Thick blood films are stained with Field A and B; these are viewed for the presence of malarial parasites.
WHO guidelines suggest three negative microscopy and antigen detection results in 72 hours to exclude malaria. In the event of a positive finding the clinician/ward will be informed. A percentage parasitaemia is only given in cases of Plasmodium Falciparum, Plasmodium Knowlesi and Plasmodium Malariae.
Please note: negative films do not exclude a diagnosis of malaria blood films and should be repeated if clinically indicated. If there has been travel to the Asia-Pacific region and clinical indication, please repeat in 12-24 hours to rule out presence of Plasmodium Knowlesi.
Assay Limitations:
- Samples more than 24 hours old may show morphological changes to the parasites and red cells due to sequestrene effect, most pertinent being the possible development of spiking on the red cells which may be confused with the fimbriation which occurs in P. Ovale infection.
- It is very difficult to detected very low quantities of parasites.
- P. Knowlesi is extremely difficult to distinguish morphologically from P. Malariae.
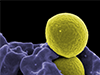
Antigen Kit
This is an immuno-chromatographic test using monoclonal antibodies against the metabolic enzyme pLDH (parasite Lactate Dehydrogenase) and HRP2 (Histidine-Rich Protein 2)of Plasmodium species.
There are two monoclonal antibodies used, one specific for Plasmodium (P) falciparum, and one pan-specific antibody that reacts with all four species found in humans:
P falciparum, P. ovale, P. vivax and P. malariae.
Assay Limitations:
- The presence of P.knowlesi cannot be excluded or confirmed with this kit.
- ovale, P. vivax and P. malariae cannot be distinguished from one another.
- Cannot distinguish P.falciparum infections from mixed infections that include P.falciparum, this highlights the importance of undertaking microscopy in parallel.
- This is not a quantitative test
- Sensitivity falls at low parasitaemia - Especially at <200 parasites/µl
- A positive control is not commercially available for this test therefore batch acceptance is not possible.
- Non-specific reactions can be caused by using samples that are not tested within the sample stability timeframe.
- The test procedure, precautions, and interpretation of results for this test must be followed when testing. Reagents from different lot numbers must not be mixed.
- The test should be used within 15 minutes after removal from the pouch to prevent exposure to humidity.
- The strips should not be frozen.
False Positives
- The presence of rheumatoid factor which can cause false positivity has previously been reported with the diagnostic devices based on the detection of HRP II (Grobusch et al, 1999).
- Detection of HRP2 of P.falciparum can give positive results for up to two weeks following treatment even after parasite clearance has been confirmed by microscopy.
- Antigen may sometimes be detected after the infecting parasites have died following treatment or due to the persistence of malaria gametocytes which do not cause illness.
- Rapid diagnostic tests cannot distinguish between sexual and asexual stages of malaria. Thus, patients adequately treated for malaria and with only gametocytes in their peripheral blood may still give a positive RDT result. Gametocytes are not pathogenic, and gametocytes of P.falciparum can persist following treatment implying drug resistance. As the persistence of antigen in successfully treated patients does not correlate with microscopy or with symptoms, these rapid diagnostic test results are considered false positives.
Corrective Action: If suspicion of malaria remains high, the assay should be repeated within 12-24 hours and these assays should always be performed in parallel with blood films.
False Negatives
- A prozone effect. This is where a high concentration of antibody may mask the antigen making it unavailable to be detected in the rapid assays.
- The presence of a mutation or deletion within the HRP2 gene.
- The kit is not extensively evaluated against P.knowlesi, therefore a negative test result, does not exclude an infection.
Corrective Action: When the clinical suspicion of malaria remains high despite a negative rapid diagnostic test result, the assay should be repeated within 12-24 hours and these assays should be performed in parallel with blood films. The possibility of concomitant non-malarial illness in cases which parasites have been demonstrated should also be considered.
Specifications
- EQA Status: NEQAS
- EQAS Scheme: Yes