Vitamin B1 and Vitamin B6 B1, B6
Specimen Volume
Minimum of 1 mLSpecimen Transport
FrozenSample Preparation
Turnaround Time
2 to 3 weeksSample Processing In Laboratory
Samples should be protected from light (do not separate) and then stored frozen.Sample Stability
Light-protected whole blood samples can be stored at room temperature for 3 hours. After 3 hours, they must be stored in the fridge (4°C) and are stable for 5 days. For longer storage, samples should be frozen (3 months).General Information
Vitamin B1
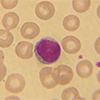
Vitamin B1 (syn. thiamine) is found inside erythrocytes where its in active form, thiamine pyrophosphate (TPP). TPP is an important cofactor for enzymes involved in metabolic processes including pyruvate dehydrogenase, oxoglutarate dehydrogenase, branched-chain amino acid dehydrogenase and transketolase. Vitamin B1 is excreted via the kidney after dephosphorylation to the free form or as a conjugated sulphate ester.
Vitamin B1 deficiency is commonly associated with malnourishment/low intake (eg, in alcoholics, elderly), severe vomiting, increased requirements (exertion, pregnancy, fever, breast feeding and rapid adolescent growth) or increased loss (haemodialysis). Deficiency of B1 causes a sensory polyneuropathy and/or decreased muscle weakness (dry beri-beri), cardiac failure (wet beri-beri), Wernicke’s encephalopathy, which is characterised by confusion, loss of muscle coordination and double vision. Wernicke’s encephalopathy can progress to Korsakoff’s syndrome, of which memory loss and hallucinations are key features. The most common presentation is encephalopathy, which is most often observed in patients with chronic alcoholism.
Toxicity resulting from high doses of vitamin B1 has not been described, except for occasional instances of non-immune anaphylaxis.
Vitamin B6
Vitamin B6 encompasses three naturally occurring pyridine derivatives: pyridoxine, pyridoxamine and pyridoxal, as well as their 5-phosphate esters. The main circulating forms of vitamin B6 are pyridoxal (PL) and pyridoxal 5’- phosphate (PLP). These two forms are detectable in both plasma and red blood cells. The functional form of vitamin B6 is PLP. Vitamin B6 is sourced from the diet and excreted through the kidneys as pyridoxic acid.
PLP is a coenzyme for many enzymes in the body, for example decarboxylases, aminotransferases and glycogen phosphorylase, and therefore plays a key role in the metabolism of proteins, carbohydrates, fats and homocysteine. It is also important for the synthesis of haem and several neurotransmitters (eg, serotonin, dopamine, epinephrine, norepinephrine, and γ-aminobutyric acid).
Symptoms of vitamin B6 deficiency are skin changes, such as scaling or hyperpigmentation, as well as brain-specific symptoms such as irritability, depression, and dementia. Because of the direct involvement of vitamin B6 in the conversion of the amino acid homocysteine to cysteine, vitamin B6 deficiency leads to a rise in homocysteine and an increased risk of atherosclerosis. Anaemia (normocytic, microcytic or sideroblastic) can also occur because iron absorption is restricted.
At risk groups include patients with CKD, malabsorption, homocystinuria (can cause vitamin B6 deficiency), certain medications, such as antiepileptic drugs, and ethanol excess. However, specific vitamin B6 deficiency is rare; it usually occurs in combination with other water‑soluble vitamin deficiencies because of malabsorption states, increased losses (eg, during renal dialysis) and as a result of inadequate nutrition. PLP is mainly bound to albumin in the plasma and so concentrations can fall in the presence of systemic inflammatory response independent of vitamin B6 nutritional status.
Chronic high doses of vitamin B6 supplements have been linked to sensory neuropathy and dermatological lesions.
From June 2005 we have discouraged service users from requesting red-cell transketolase unless there is a particular requirement in which case this must be discussed with the Duty Biochemist. Note that transketolase activity is only stable for up to 2 weeks at -20 degrees.
Patient Preparation
Patients should be fasted and the sample collected in the morning prior to any medication. Avoid measurement of vitamin B6 during a severe acute phase response eg surgery, allowing at least 14 days afterwards.
Reference Range
Vitamin B1: 66.5 to 200 nmol/L
Vitamin B6: 44 to 168 nmol/L
Source of Reference Range
KitSpecifications
- EQA Status: INSTAND
- EQAS Scheme: Yes