Bilirubin (Total) (TBil)
Specimen Volume
1mL blood (~250uL sample)Turnaround Time
24 hoursSample Processing In Laboratory
No special requirementsSample Stability
7 days at 2-8°C.General Information
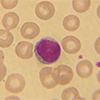
Bilirubin is formed in the reticulo-endothelial system mainly the spleen, when aged erythrocytes are degraded. Haem from haemoglobin and other haem-containing proteins is converted to bilirubin, bound to plasma albumin and transported to the liver (unconjugated or indirect bilirubin). In the liver, it is conjugated with glucuronic acid for solubilisation (conjugated or direct bilirubin) and transported through the bile duct for elimination via the digestive tract. Increased bilirubin in the circulation gives rise to jaundice.
Unconjugated bilirubin is increased when diseases or conditions produce bilirubin faster than it can be metabolised e.g. liver immaturity. Bile duct obstruction or damage to the hepatocellular structures lead to increases in both conjugated/direct bilirubin and unconjugated/indirect bilirubin.
Patient Preparation
No special patient preparation
Reference Range
<21 μmol/L
Source of Reference Range
Pathology HarmonySpecifications
- EQA Status: UK NEQAS Clinical Chemistry Scheme
- EQAS Scheme: Yes