Cellular Pathology - University Hospitals Birmingham
Cellular Pathology is based across UHB sites at QE Hospital Birmingham, at Birmingham Heartlands Hospital, Solihull Hospital and at Good Hope Hospital.
The majority but not all of Cellular Pathology tests that are performed and equipment in use are accredited to internationally recognised standards for medical laboratories ISO 15189. This is important for the Department and for service users as it provides assurance on quality and competence. There is increasingly an integrated approach across the different UHB hospital sites where staff, equipment and testing may be shared to deliver the highest possible quality services to our service users. The full range and nature of accredited tests is detailed on the United Kingdom Accreditation Service website https://www.ukas.com 10141 Schedule of Accreditation .
The Department is currently supporting the Trust with significant increases in clinical activity. For some specialties reporting times have fallen bellow targets and so the Department is working with service users to minimise the impact of this. The Department is prioritising clinically urgent requests and patients on cancer pathways, recruiting and working additional sessions. The Department is also outsourcing reporting of some requests to two external specialist UKAS Accredited suppliers that hold contracts with the Trust.
Specialist Services within Cellular Pathology (by site), QE=Queen Elizabeth, BHH=Birmingham Heartlands, SH = Solihull, GH=Good Hope
- MOHS (QE, SH) - microscopically controlled surgery used to treat common types of skin cancer.
- Neuropathological Smears (QE) - rapid diagnostic service for intra-operative brain tissue specimens
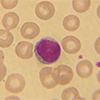
- Cytopathology (BHH,QE) - diagnostic cytopathology services for the Trust including fine needle aspirations, endoscopic brushings and washings, EUS-FNAs , serous fluids urines and CSF.
- Muscle Biopsy Service (QE) - part of the investigation of a clinically suspected neuromuscular disorder when other less invasive tests have not provided a firm diagnosis.
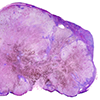
- Electron Microscopy (QE) - used routinely at magnifications of between 1500 and 70,000 times to examine the ultrastructure of cells and their surroundings.
- Andrology (GHH) - Diagnostic, Post Vasectomy and Retrograde Semen analysis . The service operates from a single site located on the 1st Floor of the Sheldon Unit at Good Hope Hospital.
- Direct Immunofluorescence (BHH and QE) - Direct immunofluorescence is used for the detection of tissue bound proteins such as antibodies and complement proteins. Two types of tissue, skin or renal, are processed, This method allows for the detection of tissue bound antibodies when there may be insufficient levels to detect in serum.
- Mortuary (QE, BHH, SH, GH) - Body storage available on all sites with 10 freezer storage spaces available on the Solihull sites and 16 on the QE site. Post Mortems can be carried out on the Heartlands and QE sites.
- Immunohistochemistry (QE, BHH) - carried out using different platforms and antibodies across the sites. See attached UKAS scope for those antibodies accredited. At present there are a few antibodies that are not yet accredited but will be added to the scope in due course.
Minimum Dataset required for Cellular Pathology Requests
In order to process specimens it is essential that request forms are fully completed in a clear and legible format. The use of patient ID stickers is permitted however please ensure you use the full patient sticker NOT the smaller blood tube sticker. All specimens received into Cellular Pathology must meet the agreed laboratory minimum dataset; any specimens not meeting the criteria will be returned to the requesting department. Please ensure that any important information (e.g. clinical history, bleep number etc.) is clearly indicated on the form and ensure that any priority or urgent cases are marked as such.
- Trust users can make request via a theatre request book entry or by completing an internal UHB histopathology / cytopathology request form.
- GP and dental practices should complete the external request form which can be supplied on request from the Department and for internal service users this link http://www.uhb.nhs.uk/gps/laboratory-information/ shows this request form together with specific request forms used within the Trust (QE site) for liver and breast biopsy cases. For Heartlands, Good Hope and Solihull users then request forms are available from the Department of via a request to This email address is being protected from spambots. You need JavaScript enabled to view it.
TWO unique patient identifiers must be present on both the request form and specimen container i.e. a minimum of the PID, NHS number or the DOB together with the patient surname and forename/initial in order to be accepted by the department. Other missing data (e.g. full clinical details) may be clarified over the phone or by email as needed.
Sample pot requirements
- Patients full name (or as a minimum; surname with initial)
-
Hospital or clinic PID / NHS no. AND/OR Date of birth
Request form
-
Patient’s full name.
-
Date of birth.
-
Hospital or clinic PID / NHS no.
-
Address
-
Location
-
Clinical details
-
Request form must be signed
-
Consultant / GP
If one or more than one specimen is taken from the same patient the specimen containers and request form must be clearly labelled with the sites of the spec and indicated as parts 1,2,3 etc.
Hazardous Specimens
Specimens arising from patients with known or suspected transmissible diseases (e.g. tuberculosis, viral hepatitis, HIV) must be clearly labelled as such to prevent unnecessary risk to laboratory staff.
Specimen Containers
When requesting stock a member of staff from the Cellular Pathology department will inform the requestor when they will be ready for collection by the portering staff. Consumables provided by the lab should be transported via the porters so please allow time for preparation and transport. External requests for sample pots and request forms are through contacting the Department. For Heartlands site please e-mail This email address is being protected from spambots. You need JavaScript enabled to view it., for QE site use This email address is being protected from spambots. You need JavaScript enabled to view it..
Transportation of Specimens
Specimens are collected at regular intervals from theatres and all relevant departments via portering services. Urgent and unfixed (dry/not in formalin) specimens should NOT be left until the next routine collection – telephone portering services and arrange for a member of staff to bring the sample(s) to the laboratory without delay.
Please note specimens must be despatched to the Department within a secondary bag or secure transport box with sufficient absorbent material to absorb/contain any potential spillage. Formalin is a hazardous reagent with any leakages put portering, transport and laboratory staff at significant risk. Please ensure containers are closed or sealed with appropriate fitting lids. If in doubt please seek advice from the Department.
Urgent Reporting
Occasionally it may be necessary for a requesting clinician to highlight a specimen as clinically urgent. If an urgent report is required it should be clearly identified or indicated on the request form. Urgent requests should be sent to Cellular Pathology via the porters without delay.
To ensure that cases are not delayed within the laboratory please make sure that the request form is correctly completed and all sections are filled in properly. Once received urgent cases will be highlighted by the specimen reception and prioritised appropriately in the departmental workload.
In addition to clinically urgent cases there are UHB wide @FDS@ or Faster Diagnosis Specification stamps to fast track these patient cancer samples. This is to support end to pathways and prevent patient breaches where possible through prioritisation.
Service Background
The Department of Cellular Pathology provides a diagnostic histopathology, cytopathology, andrology, muscle biopsy, electron microscopy, Mohs, post mortem and mortuary service to internal users (other Trust departments e.g. surgery) as well as external users (GPs, dental and private practices). The Department also incorporates the Tissue services for the Trust; this Department is responsible for managing and ensuring compliance of the licensable activities which falls under the HTA Human Application Sector, this includes procurement, testing, storage, traceability, disposal and distribution of human tissue and cells for therapeutic use.
Cellular Pathology Department operates within the Quality Management System for Pathology Services and is led by a Clinical Service Lead Dr Bruce Tanchel. A technical Service Manager, Head Biomedical Scientist, Saeeda Kauser oversees the management of the Department. Cellular Pathology participates fully in UK NEQAS External Quality Assurance schemes where appropriate. The Laboratory works to ISO 15189 requirements and is assessed by UKAS to evaluate compliance. The vast majority of equipment, procedures and tests offered by the Department of Cellular Pathology are included in the UKAS scope of Accreditation seen here: https://www.ukas.com schedule 10141 . Some non-accredited tests may also be used to support diagnostic tests and these are mainly reflected in stains, antibodies and associated platforms that are currently under assessment by UKAS for potential additions to the scope of laboratory testing.
Some non-gynae cytology remains available at the QE Laboratory site but the majority of cytology samples across UHB are transferred to the Heartlands Hospital site for processing and staining. The routine histopathology repertoire includes specialist renal, liver, muscle and nerve processing and reporting and a well established electron microscopy service.
The Department provides a comprehensive pathology service to the Trust, South Birmingham Community and Mental Health Trusts, Private Hospitals, General Practitioners and General Dental Practitioners. The core laboratory sites are open Mon-Fri between 08:00 and 17:30 with QE Cell Path also open Sun 07:00-15:00 and Heartlands Cell Path Sat 09:00-12.45. A specialist/expert referral service is also provided to hospitals in the West Midlands, nationally and to international clients.
The Department operates within the Quality Management System of the Clinical Laboratory Services and is led by both a consultant medical Clinical Service Lead and a technical Service Manager. Cellular Pathology participates fully in UK NEQAS External Quality Assurance where appropriate.
Cellular Pathology currently employs 32 consultant pathologists who cover a broad spectrum of clinical specialities, MDTS and are also available to offer clinical advice and interpretation of results if required. Consultants can be contacted for specialist clinical advice by contacting the Cellular Pathology Offices on the QE (0121 371 3326) and BHH (0121 424 3884) sites.
Personnel
|
Cellular Pathology Department |
Good Hope, Heartlands and Solihull Team Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 1188, ext. 41188 Queen Elizabeth Hospital Birmingham Team Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3326, ext. 13326 Bone and soft tissue tumour unit This email address is being protected from spambots. You need JavaScript enabled to view it. |
|
Clinical Service Lead - Cellular Pathology Dr Bruce Tanchel |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 2196 |
|
Human Tissue Authority Designated Individual Dr Gerald Langman (Post Mortem Licence – SH/BHH/GH/QE) |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 3189 |
|
Cellular Pathology - Head Biomedical Scientist Saeeda Kauser |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3343 |
|
8a Operational Managers /Deputy Head Biomedical Scientists - cross site roles include: Becci Taylor Cytology, Andrology and Office Lead Jane Gilbert Main Lab Lead Gavin Rock IHC/Special stains Lead Rizwan Qamar Dissection/Bone & Soft Tissue Tumours Bev Whitehouse Electron Microscopy Lead |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Specific contacts as below: Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3336 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 3188 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 0189 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3352 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 5720 |
|
Mortuaries |
Good Hope enquiries Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Heartlands and Solihull enquiries Email: This email address is being protected from spambots. You need JavaScript enabled to view it. QE enquiries Email: This email address is being protected from spambots. You need JavaScript enabled to view it. |
|
Mortuary Manager / Quality lead Katie Goodall |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel QEHB: 0121 371 2520/2523 Tel BHH: 0121 424 2197 |
|
Tissue Services (Human Applications) Alexandra Martin |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 6838 |
|
Quality Lead Samantha Hoccom (QE Based) Joanne Small (BHH Based) |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 5968 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 3832 |
|
Training Lead Hannah Mckenna (Cross site) Tracy Bright (QE based) |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 1191 / 0121 371 3314 Email: This email address is being protected from spambots. You need JavaScript enabled to view it.This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3314 |
|
Health and Safety Lead Rizwan Qamar Joanne Small |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3314 Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 3832 |
|
Muscle Service Ferhana Maqsood |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 5720 |
|
Andrology Emma Whitehouse |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 9717 |
|
Cytology Shabnam Latif |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 424 1191 |
|
Electron Microscopy Beverley Whitehouse |
Email: This email address is being protected from spambots. You need JavaScript enabled to view it. Tel: 0121 371 3352 |
Specimen requirements
Due to the wide range of cellular pathology specimens several key container types exist as below. The size of the specimen container must be appropriate to the size of the specimen.
|
Specimen Type |
Container |
|
Small specimens |
Yellow Topped 60 mL Containers for biopsies and small resection e.g. skin ellipses, appendicies. |
|
Routine specimens |
350 mL White Topped “Honey Pots” - Suitable for larger specimens e.g. gall bladders, larger skin resections femoral heads These pots are also suitable for biopsy specimens where the tissue is adhered to glass microscope slides. |
|
Large resection specimens |
Specimen buckets without fixative / dry - Fixative is supplied to theatres from pharmacy and is added to the container with the specimen prior to sending to the histology laboratory. e.g. bowel, heart, breast tissue. |
|
“Mega” Specimen Buckets |
The buckets should be collected from cellular pathology in advance of the surgery taking place. Specimens MUST NOT be placed into yellow clinical waste bags or Griff Bins as these WILL NOT be opened by laboratory staff and should ONLY be used for the incineration of clinical waste. Large anatomical or specimen resections e.g. large sarcomas. |
|
Dry Samples (Within Lab hours only) |
Specimen buckets, 60ml pots / Theatre Tissue Safe system. Dry samples sent to the lab e.g. frozen sections; MOHS samples: lymph nodes; Research projects/biobank samples |
|
Cytopathology Specimens |
|
|
Urine |
A universal container. |
|
Smears kits |
Microscope slides; slide carriers; spray fix and cytorich red needle wash containers. |
|
Serous Fluids/ Sputum/ respiratory fluids/CSFs |
Universal Containers. Do not use glass containers. |
To ensure that cases are not delayed within the laboratories please make sure that the request form is correctly completed and all sections are filled in properly. Once received urgent cases will be highlighted by the specimen reception and prioritised appropriately in the departmental workload.
Please note many of the technical preparation aspects of cytology may take place at the Heartlands Hospital Cell Path Laboratory.
Intra-operative Frozen Sections
The department provides a rapid diagnostic service for intra-operative tissue specimens. Requests for frozen section should be telephoned to the histopathology laboratory (at QE site 0121 371 13314 and at BHH site 0121 424 3188 ) in advance of the procedure being undertaken, preferably on the day prior to surgery. Where this is not possible, e.g. an incidental finding during surgery, the request should still be telephoned to the laboratory prior to the sample leaving theatre. When calling the laboratory please ensure that you have the following information available as it will be asked for by the person receiving the call:
-
Patient’s full name.
-
Registration number.
-
Date of birth.
-
Contact number or bleep number.
-
Patient’s consultant.
-
Tissue type / nature of specimen.
-
Expected date and time of delivery to the Lab.
Tissue taken for frozen section should be placed into a suitably sized container without any form of fixative (i.e. dry) and sent in a secondary bag/container to Cellular Pathology without delay. The transport of the fresh material is arranged by the requesting clinical team, typically using a UHB Hospital porter. Theatre books should be used to record the audit trail from theatre and safe receipt in the laboratory. The process from specimen receipt in the laboratory to verbal report issued takes 15 to 30 minutes however this time may be shortened or lengthened slightly based on the nature of the sample received. High risk biohazardous tissues are not suitable for frozen sectioning unless absolutely clinically required. Examples of these include tuberculous lesions, specimens from patients with viral hepatitis and specimens from patients who are HIV positive. If there is any doubt as to whether the specimen is suitable or not please contact the laboratory and ask for the advice of a Consultant Pathologist.
Immunofluorescence
Instructions for Collection of Samples
Do NOT Put Samples For IMF in to Formalin
Skin Samples
Skin samples are wrapped in saline soaked gauze and place in a universal container with full patient details label attached. The skin samples must include the dermal-epidermal junction (DEJ) for tests to be performed.
Renal Samples
Renal samples are placed in saline solution in a universal container with full patient details label attached. Renal samples must include the portion of a kidney containing glomureli.
Any other tissue sample requiring IMF must be placed in saline. Formalin is NOT an appropriate medium; IMF tests cannot be performed on formalin fixed tissue.
Sending samples to Cellular Pathology department
Samples from patients with known infectious risks ie. Hep B, TB, HIV must be discussed with a pathologist or Immunologist before the sample is taken.
Fill out a Histology form with all the patient and corresponding clinical details. The form must be clearly labelled IMF.
If a sample for routine histology has been taken alongside the IMF sample then one form can be sent detailing the pots and instructions for tests needed. All samples taken on one patient are to be sent together (thus one uniform report can be generated).
Samples requiring IMF analysis must be sent as soon as possible, within 24 hours of collection to ensure optimal results.
MOHS
Mohs, is microscopically controlled surgery used to treat common types of skin cancer. During the surgery, after each removal of tissue and while the patient waits, the fresh tissue is snap frozen and sectioned for microscopic examination. The examination informs the decision for additional tissue removal.
The process from specimen receipt in the laboratory to verbal report issued takes no longer than 15 minutes per sample block however complex specimens with multiple samples will take additional time.
Mohs clinics are booked with the Department to ensure that there are clinical and technical staff are available to complete the test. Mohs surgery is carried out at Solihull and QE Hospital sites.
Neuropathological Smears
The Department provides a rapid diagnostic service for intra-operative brain tissue specimens. Requests for neuro smears should be telephoned to the laboratory in advance as per intra-operative frozen sections.
Tissue taken for neuropathological smears should be placed into a sterile universal container (UC) without any form of fixative (i.e. dry) and sent to Cellular Pathology without delay. These specimens are often tiny and so any delay in receipt may lead to artefactual damage which can be detrimental to any further laboratory processing.
The process from specimen receipt in the laboratory to verbal report issued takes 15 - 30 minutes however this time may be shortened or lengthened slightly based on the nature of the sample received.
Small Biopsy Specimens
The Department provides both a routine and urgent diagnostic service for small biopsy specimens.
Specimens should be placed into 60 mL pre-filled containers of neutral buffered formalin.
-
Wherever possible small or endoscopic biopsies should be placed into mini biopsy or microcassettes cassettes (small yellow cassettes) before being placed into the neutral buffered formalin pots. Supplies of cellsafe cassettes can be sourced from the Cellular Pathology Specimen Reception.
-
Breast or other fine cores may be placed onto white cards before being placed into neutral buffered formalin pots. Please ensure the cores are stretched out linearly prior to fixation as knotted cores are not easy to separate out in the laboratory.
Please note that biopsies are delicate and should be handled with care, avoid the use of forceps wherever possible to prevent trauma artefact to the tissue.
Urgent Biopsy Specimens (Rapid Paraffin Service)
The Department provides a rapid paraffin service for clinically urgent biopsy specimens; a report can be issued on the same day that the specimen arrives in the department. It should be noted however that not all specimens are suitable for rapid processing. In general terms only liver, renal and cardiac biopsies are processed in this way. Other specimens may be suitable however advice should be sought from the Histopathology Manager (0121 371 3352) or a trimming room senior Biomedical Scientist (0121 371 3314) prior to sending other tissue types.
Tissues for the rapid paraffin service must be received by the department no later than 13:30. Please ensure that the name and bleep number of the requesting clinician is clearly indicated on the request form to allow for the verbal report to be issued.
Specimens received after 13:30 will not be processed urgently and will be placed onto the “normal” biopsy run later in the day thus same day reporting will not be possible.
Resection Specimens
The department provides a routine and urgent diagnostic histopathology service for larger surgical resection specimens. Tissue should be placed into appropriately sized containers which will allow for the specimen and at least ten times its volume in fixative (i.e. neutral buffered formalin) to be contained.
DO NOT use containers which are too small to allow for this volume of fixative to be used or squash specimens into small pots. Specimens should be free-floating in fixative not pressed up against the sides of the container as this leads to distortion of the tissue and may make further processing unnecessarily difficult.
Reporting
Once specimens are reported and authorised by the laboratory they can be accessed on the intranet by appropriate staff. In addition a typed copy will be sent to the destination specified on the request form (FOR EXTERNAL USERS ONLY). If the specimen is needed for a particular MDT or clinic, then please state this on the request form. Urgent reports can be issued verbally if necessary to a suitable member of medical staff. Please put a mobile telephone number or a bleep number (that will be answered immediately) on the request form. Telephone reports will only be issued on request via telephone.
Laboratory Turnaround Times
The Department monitors turnaround times on a regular basis and reviews significant delays or service issues within the Trust's Divisional Diagnostic Performance monthly meetings. 7, 10 and 14 day Cellular Pathology turnaround target reporting times are reported to Trust service users, broken down by clinical specialty for biopsies and for cancer tracking cases for each month. Specific turnaround data is available to service users upon request in addition to UHB internally available histopathology intranet dashboards. The agreed routine TATs for each specialty is 14 days to first reported for greater than or equal to 90% of cases, within tolerance = 75% - 90% reported in 14 days. Targets for reporting are not consistantly met, but of note is some more complex haematopathology and urology cases may require additional work e.g. immunohistochemistry or molecular pathology and this does add to reporting times for complex cases.
In addition the Department actively monitors outstanding cases, notifying reporting pathologists that cases are still unreported. This and actions to increase lab and consultant capacity continue to support the delivery of improved TATs for service users.
Muscle Biopsy Service :
- Histochemistry results is 7 days
- The current turnaround time for cases referred to specialist centres is 2-3 months depending on tests requested.
Electron Microscopy :
- Renal and cardiac turnaround times are approx. 10 to 14 days, TATs may be longer with a small specialist EM team
- Muscle and nerve biopsies approx. 10 to 14 weeks.
Referral Laboratories and second opinions
For some complex cases outside, second opinions may be requested internally within UHB but also externally to support the diagnostic report and this may add to the number of days before a final diagnostic report is issued. List of key contacts we currently use for specialist second opinions and referral labs used for testing is available upon request.
Unaccredited testing
The Department regularly reviews testing to reflect clinical service needs and advances in technology. Consequently, some testing and equipment has not yet been reviewed at UKAS assessment visit. The following testing and aspects of Cellular Pathology are not covered by UKAS 15189 accreditation:
Sputum Analysis - Differential cell count performed on induced and non-induced sputum samples. A developmental diagnostic tool to deliver accurate severe asthma diagnosis and phenotyping. This will be a step towards patient tailored medicine delivery in severe asthma and will enhance our Trust position as a leading national centre in the management of severe asthma.
Digital Pathology - The Department is performing extensive clinical validation towards going live with digital pathology in 2024. 3D HISTECH - PANNORAMIC 480, Hamamtsu S60 and S360 slide scanners are used as part of a Sectra IDS7 software solution for viewing and reporting digital images. This will be subject to a UKAS 'Extension to accredited scope' application later. To enable this PACS reporting went live during 2024. Therefore some cases are reported using this system and this is not within our scope of accreditation.
UHB, Department of Cellular Pathology
- Created on .
- Last updated on .
- Hits: 10495