Suitable Specimen Types
CSFCSF Xanthochromia
Specimen Volume
1 mL (min.vol of 160 uL), a serum sample for bilirubin and total protein should also accompany the CSF sampleSample Preparation
- Label request form with CSF sticker and complete.
- The CSF should be centrifuged at >2000 rpm for 5 min ASAP after receipt, ideally within 1h of collection.
- Store in the dark at 4oC until analysis is performed.
Turnaround Time
4 hoursSample Processing In Laboratory
A.S.A.P but DO NOT use post tube system.Samples must be protected from light.
Sample Stability
4°CGeneral Information
Subarachnoid haemorrhage (SAH) is spontaneous arterial bleeding into the subarachnoid space, usually from a cerebral aneurysm. Patients who have bled, and in whom the diagnosis is initially missed, often present with a further bleed, in a poorer condition and with a worse outcome than in those in whom the correct diagnosis is made promptly. It is thus crucially important to detect SAH in all patients in whom it has occurred.
The initial investigation of choice is a CT scan which in experienced hands will show blood in approximately 93% of patients presenting within the first 24 h after an event. Detection rate falls with time to about 50% in patients presenting after 1 week. Patients with a positive CT have cerebral angiography to confirm the presence of an aneurysm and locate its site. This invasive procedure carries with it a small but definite risk of morbidity and mortality. There is thus a need for a procedure for detecting those 2-5% of CT negative patients presenting with a history suggestive of SAH, who actually have sustained a SAH, and for eliminating the diagnosis in the remaining 95%-98% without the need for angiography.
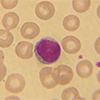
Following haemorrhage into the CSF, red blood cells undergo lysis and phagocytosis; the liberated oxyhaemoglobin is converted in-vivo in a time-dependent manner into bilirubin, and sometimes methaemoglobin. Of these three pigments, only bilirubin arises solely from in-vivo conversion. Oxyhaemoglobin (and possibly methaemoglobin) may both be produced prior to, but also during or after, CSF sample collection.
Bilirubin may be detected in CSF by spectrophotometry or by visual inspection for the yellow discoloration (xanthochromia) it imparts to CSF. Evidence clearly indicates that visual inspection is not a reliable method and should not form the basis of any report on CSF examination. Spectrophotometry is of particular value in the investigation of CSF with an increased erythrocyte count as there is no other reliable way for distinguishing between SAH and a traumatic tap. It is also of value in the investigation of CSF with a normal red cell count from a patient presenting several days after an event by which time the cells may no longer be present.
Patient Preparation
Patient should have had a CT scan performed prior to this investigation. Proceed to CSF tap on CT negative patients only. CSF sample should not be collected until 12hrs post onset of headache.
A blood sample for measurement of serum bilirubin and total protein is also advised. It is advisable to send one of the later draw samples of CSF to Biochemistry (3 or 4) since there is likely to be less blood staining due to traumatic tap.
Do not transport specimen in pneumatic tube.
Notes
- Specimens must be collected sequentially even if no other investigations are required. The specimen for spectrophotometry should always be the last fraction to be taken, and ideally at least the fourth.
- The specimen must be centrifuged and separated within one hour of collection and protected from light prior to analysis (therefore samples from Microbiology are unsuitable for this analysis).
- Pneumatic tube systems should not be used to transport the specimen to the laboratory.
- A simultaneous blood specimen should be taken for serum bilirubin and total protein measurement.
- Record the timing of sampling relative to that of possible haemorrhage.This should be no less than 12h after onset of symptoms.
Heavily blood stained specimens are invalidated due to presence of serum bilirubin.
Reference Range
An interpretive comment is provided by the laboratory based on the National Guidelines for Interpretation of CSF Spectrophotometry.
Specifications
- EQA Status: IMMQAS
- EQAS Scheme: Yes